Learning objectives
|
Introduction
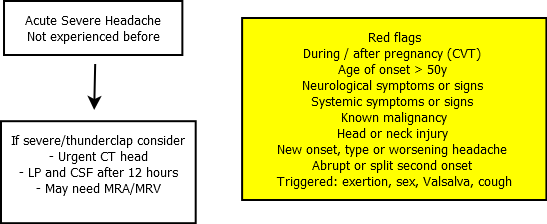
Acute headaches without any concerns of underlying brain pathology i.e. Primary headaches will rarely come to the attention of stroke physicians other than migraine. Migraine with aura is a common cause of associated headache with transient focal neurology and will be discussed below. Thunderclap headaches with sudden onset and intensity peaking within 1 minute should always raise the concern of SAH and these patients need an urgent CT head which is over 99% sensitive if done early. If there is a severe headache and lateralising neurology and no blood on CT then this is likely an ischaemic event. With modern scanners and early scanning CT is incredibly sensitive at diagnosing SAH. Occlusion of a large artery e.g. MCA will often cause an ipsilateral vascular type headache possibly due to increase collateral flow. These patients need urgent consideration for thrombolysis +/- Mechanical thrombectomy once a CT head has excluded any haemorrhage. Depending on the criteria for "thunderclap headache approximately 11-25% patients presenting with thunderclap headache have SAH.
| Thunderclap headache (TCH) is a sudden severe headache that peaks to maximum intensity within 1 minute. |
| Red flags for Headache |
|---|
|
| Useful clinical pointers |
|---|
|
Differential diagnosis of Acute/Thunderclap Headache
Priorities must be assessed with attention to the seriousness so that SAH, CVT, Stroke and Meningitis and pituitary apoplexy or even CO toxicity need considered and excluded first of all. For those with Thunderclap headache and normal CT and LP the prognosis is very good.
| Causes | Details | Seriousness |
|---|---|---|
| Subarachnoid Haemorrhage | red flags - worst ever headache, neck stiffness, meningism, vomited, onset with exercise. Rupture of an aneurysm or AVM is usually catastrophic and presents with thunderclap headache and often collapse and coma | Potentially Life threatening |
| Acute Stroke | both ischaemic and acute haemorrhagic stroke can cause sudden headache but more common with haemorrhage. CT scan will be diagnostic for haemorrhage. Particularly worrying is patient on anticoagulation or with any focal neurology. In those with ischaemic stroke it is often on the affected side and is a vascular headache which represents shunted blood through collaterals due to a major arterial obstruction, e.g. MCA occlusion. Needs urgent CT head | Potentially Life threatening |
| Cerebral Venous Sinus thrombosis | consider this within the differential of thunderclap presentation. CT head may be normal, show clot or venous infarction +/- haemorrhage. Suspect if LP shows high red cells, high opening pressure and increased lymphocytes. Diagnose formally with CT venography or MR venography, whichever available. Anticoagulate. | Potentially Life threatening |
| Cervical Dissection | Neck, retro-orbital pain or occipital pain. Associated focal neurological signs. Horner's syndrome with ipsilateral carotid dissection. Brainstem signs with vertebral dissection and may also have a Horner's from PICA thrombosis and lateral medullary syndrome. | Potentially Life threatening |
| Reversible Cerebral Vasconstriction syndrome (RCVS) | Reversible cerebral vasoconstriction syndrome (RCVS): single or repeated severe, often bilateral thunderclap headaches. Seizures and focal neurological deficits, ischaemic stroke and non-aneurysmal SAH, LP - blood and protein. MRA/CTA/DSA: “beads on a string” appearance of cerebral arteries which resolves at 3 months. Verapamil/Nimodipine may be given. Multiple suggested causes - idiopathic, pregnancy, vasoactive drugs, hypertensive crisis, etc. | Not Life threatening |
| Posterior reversible encephalopathy syndrome | Classical MRI appearance | Variable outcome |
| Subdural haematoma | Classical CT appearance | Potentially Life threatening |
| Epidural haematoma | Classical CT appearance. Recent head trauma then lucid period then deteriorates | Potentially Life threatening |
| Pituitary Apoplexy | severe headache and IIIrd nerve palsy and visual loss as severe pressure around optic nerve from haematoma. CT/MRI + contrast may show infarction/bleeding. May have known pituitary tumour. Needs neurosurgical decompression if vision affected. Needs IV HYDROCORTISONE because acute hypopituitarism is possible. Neurosurgical consult | Potentially Life threatening |
| Acute CNS infection | bacterial meningitis: look for petechiae if meningococcaemia, neck stiffness, Kernig's sign, meningism. Acute delirium in elderly, pyrexia. Treat empirically if any suspicion. Many with fever of recent onset and headache will have a systemic illness headache. This is poorly understood. Usually self-limiting with good outcome, when the underlying infection resolves. Some, however, end up with a non-specific persistent headache for months. | Potentially Life threatening |
| Temporal (giant cell) arteritis | subacute headache in older patient. Check ESR or CRP. Temporal artery tenderness or polymyalgia symptoms or transient or persistent visual loss. Needs TAB. | Not Life threatening |
| Acute angle closure glaucoma | consider in a patient with headache associated with a red eye, halos or unilateral visual symptoms. Urgent ophthalmology referral. | Not Life threatening |
| Carbon monoxide poisoning | CO produced when gas, oil, coal or wood do not burn fully. Cold weather. More than one person affected in shared accommodation. Check ABG and COHb levels. SaO2 falsely normal | Potentially Life threatening |
| Spontaneous intracranial hypotension | marked low pressure headache on standing. Can come on suddenly. Relieved by remaining supine. Post LP or spontaneous leak. Give fluids and simple caffeinated drinks. May need epidural blood patches (usually done by anaesthetist). Typical meningeal enhancement on MRI and cerebellar tonsillar descent and bilateral SDH. CSF opening pressure <10 cmh4O. | Not Life threatening |
| Acute Hydrocephalus | The clue may be headache, nausea and vomiting which should warrant a CT scan and then there will be evidence of ventricular dilatation and the cause may be obstructive or non obstructive. In some cases such as Idiopathic intracranial hypertension imaging may be normal and diagnosis is made by LP. It is a very strong reason for always checking opening pressure with every diagnostic LP | Can be life threatening |
| Migraine (no aura) | aura absent but severe often pulsating, often recurring unilateral headache may last 4-72 h. Shorter with effective treatment, longer than 72 h in others. Desire to be alone, quiet, lie down and sleep. Severe attack looks ill, nauseated, grey pallor. Feels very miserable. Headache often worse than those with aura. Manage as migraine with aura. | Benign |
| Migraine with aura | recurrent episodic headache with systemic symptoms. Comes on gradually, and there may be preceding aura such as tingling, weakness, and altered speech, word finding difficulties, flashing lights, scotomas or fortification spectra. Positive family history. Headache then comes on and lasts 4-72 h by definition but some are shorter and some longer. Patients feel awful; look grey, usual response for severe attacks is to want to lie down and sleep. First line: ASPIRIN 900 mg or IBUPROFEN 600 mg PO if not vomiting or else DICLOFENAC 100 mg PR + METOCLOPRAMIDE. Second line: triptans, e.g. SUMATRIPTAN 50 mg PO or 6 mg SC (C/I with IHD/TIA, stroke). If severe vomiting, consider IV NS. | Benign |
| Cluster headaches | (commonest of the trigeminal autonomic cephalgias). Occur in repeated attacks. Severe. Unilateral. Retro-orbital stabbing. Tearing, miosis, ptosis. Restless patient pacing floor. Give 100% O2 and SUMATRIPTAN 6 mg SC as the first choice treatment for the relief of acute attacks of cluster headache. Prevent with PREDNISOLONE or VERAPAMIL. Commoner in men. | Benign |
| Paroxysmal hemicranias | severe, unilateral orbital, supraorbital, and/or temporal pain, always same side, lasting 2-45 min up to 5-10 times/day. With either conjunctival injection, lacrimation, nasal congestion, runny nose, ptosis, eyelid oedema. Dramatic effect of INDOMETHACIN 150 mg daily. | Benign |
| Short-lasting unilateral neuralgiform headache attacks with conjunctival injection and tearing (SUNCT) syndrome | rare, males > females in middle age. Moderate headache lasts 1 minute. Ipsilateral conjunctival injection, lacrimation. Nasal stuffiness/rhinorrhoea and increased intraocular pressure on the symptomatic side and swelling of the eyelids. Usually frontal and periocular. Intractable to medications. | Benign |
| Medication overuse headache | must be excluded in all patients with chronic daily headache (headache >15 days per month for more than 3 m) and those using opioid-containing medications or overusing triptans are at most risk. Resembles migraine or tension type headache. Chronic analgesic ingestion especially codeine. Gradual withdrawal. Prevent with AMITRIPTYLINE or GABAPENTIN. | Benign |
| Tension headache | usually a chronic band-like headache but many variants. Rarely truly thunderclap. Often long history of similar episodes. No associated symptoms or signs beyond headache. Give NSAID or paracetamol. | Benign |
| Coital/post-coital headache | diagnosis once SAH excluded. May be experienced with orgasm. There is a real possibility that this could be SAH but it would be less likely if it has occurred several times before without incident. In future take NSAIDs prior to sex. Exclude SAH in all cases with LP/CT. Benign form is orgasmic cephalgia once SAH safely excluded. | Benign |
| Exploding head syndrome | not a true headache but can be misunderstood with poor history. Auditory hallucination that occurs whilst falling asleep - sound like a gun going off in one's head. May be unable to speak or move. Benign condition - avoid extensive investigations or treatment | Benign |
Strokes and Headaches
Strokes , even ischaemic cause acute headaches. In my early days of thrombolysis I was concerned about SAH but the clues are that the ischaemic stroke headache is usually over the side of the brain affected by the stroke and I suspect it is a vascular type headache due to rediverted flow around and acute obstructed large arterial branch of the COW via collaterals and leptomeningeal branches. CT is over 99% sensitive to SAH in the first 6 hrs and it would be most bizzare to have a raised NIHSS and for SAH blood not to be seen on modern imaging. Here are some other observations. Cerebral venous thrombosis headache is often out of proportion to the bleeding seen and that maybe a clue to warrant looking for the diagnosis.
| Headache commoner |
|---|
|
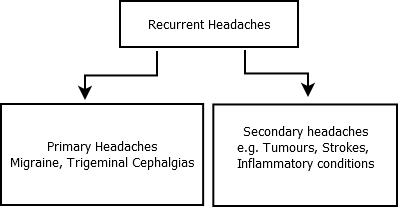
Recurrent Headaches
The prognosis of this is different though there are a few caveats. RCVS can cause recurrent thunderclap headaches. SAH can be preceded by "sentinel bleed" prior to a large bleed. However the more the headache has happened before over a long period of time with full recovery and normal imaging the more likely it is to be a primary headache
Investigations
- FBC, U&E, ESR if Temporal arteritis suspected
- CT Brain must be performed earlier and will exclude many causes. If done within 6 hrs of onset newer scanners basically can exclude SAH
- CT / CTV or MRI / MRV if Cerebral venous sinus thrombosis suspected
- CTA if RCVS suspected or with SAH in the acute setting to help localise any aneurysm
- Immediate LP and CSF with measurement of opening pressure : if encephalitis or meningitis or Idiopathic intracranial hypertension
- Delayed LP and CSF or a late SAH presentation suspected. If looking for SAH then delay until 12h. Ensure experienced operator. ALso measure pressure. Send 4th bottle for xanthochromia which is best performed using CSF spectrophotometry. Protect sample from light and get to lab quickly
| It is still true that patients who have had thunderclap headache who have a normal CT Brain and normal CSF carry an excellent long term prognosis |
Management
- ABC as ever. If comatose and unwell then once stable with intubation and ventilation if needed and then urgent CT head usually will help to define the cause and urgent need.
- If stable more time can be taken to dwell on the history and exam and need for urgent CT(A/V) and CSF sampling.
Next: >> Subarachnoid haemorrhage |
References and further reading
- Acute Headache. Ulster Med J. 2014 Jan; 83(1): 3-9. Raeburn B Forbes
- Dr Ben Wakerley Consultant Neurologist Gloucestershire Royal Hospital. Acute headache on the AMU
| Note: The plan is to keep the website free through donations and advertisers that do not present any conflicts of interest. I am keen to advertise courses and conferences. If you have found the site useful or have any constructive comments please write to me at drokane (at) gmail.com. I keep a list of patrons to whom I am indebted who have contributed. If you would like to advertise a course or conference then please contact me directly for costs and to discuss a sponsored link from this site. |