Learning objectives
|
Introduction
Depression after stroke is common. It can have a substantial effect on rehabilitation outcome and life, function, relationships and quality of life. Approximately half of all stroke survivors suffer clinical depression at some time. Many recover but have further episodes (Ayerbe et al, 2011) and 30% are clinically depressed at any one time. Probably 40% are clinically anxious at some time after stoke. 20% to 25% of survivors suffer from clinical anxiety at any one time. A stroke in many aspects resembles a bereavement and for the patient there is often a loss which takes time to accept and adjust to. Anxiety and depression are common after stroke. The most important action for staff is to explain this to patients as the impact will sometimes not hit until after discharge and they need to realise that these feelings are normal and that they should speak with the stroke team and their own General practitioner if it is affecting life. I ensure that partners are aware that the patient may be quiet, moody, short tempered and at times fairly difficult to be with. This settles with time. It can make an enormous difference knowing this in advance.
Dealing with loss
The loss can be different for many patients, functional such as an inability to do basic toileting without help and a feeling of loss of control and dignity. It may be concerns that their partner will leave them and the changing nature of a relationship. Difficulties with intimacy or sexual life. Unable to work and concerns financially. It may be the loss of an enjoyable past time that was central to their social life such as dancing. The key is to talk sensitively and empathetically with patients. There may be clues that the patient is unhappy – tears and obvious sadness and things said or simply withdrawal and a refusal to take part in usual activities. Other affects may be loss of appetite or sleeping too much or too little. One of the most impacting losses is that of speech. In most cases things do improve with time. Patients should be given realistic views - I often explain that it takes a year to get over a stroke emotionally and that is a reasonable experience. If mood is significantly impacting life and ongoing activities I will start an antidepressant and involve psychology. Suicide after stroke is rare but does happen and so suicidal ideation should be discussed. However sometimes although very rare, patients who are suicidal may deny this strongly so that they can carry out their plans.
The loss often affects others close to the patients. It may be a spouse or a parent who can no longer taxi their teenager to their usual after school activities and this can lead to resentment from others. It can be the spouse and in some cases the parent who has to help a young adult deal with their stroke. Every situation is different but there are common themes.
Exploring Issues
- Ask about any pain which can certainly worsen mood
- Frustration and feelings of isolation.
- Impacts of reduced mobility
- Impacts of reduced vision - diplopia and hemianopia
- Relationship and sexual issues
- Financial issues
- Issues over employment
- Dysphasic patients feeling stupid, isolated, frustrated
- Toileting and dignity issues
- Difficulty with feeding and nutrition
Screening tests
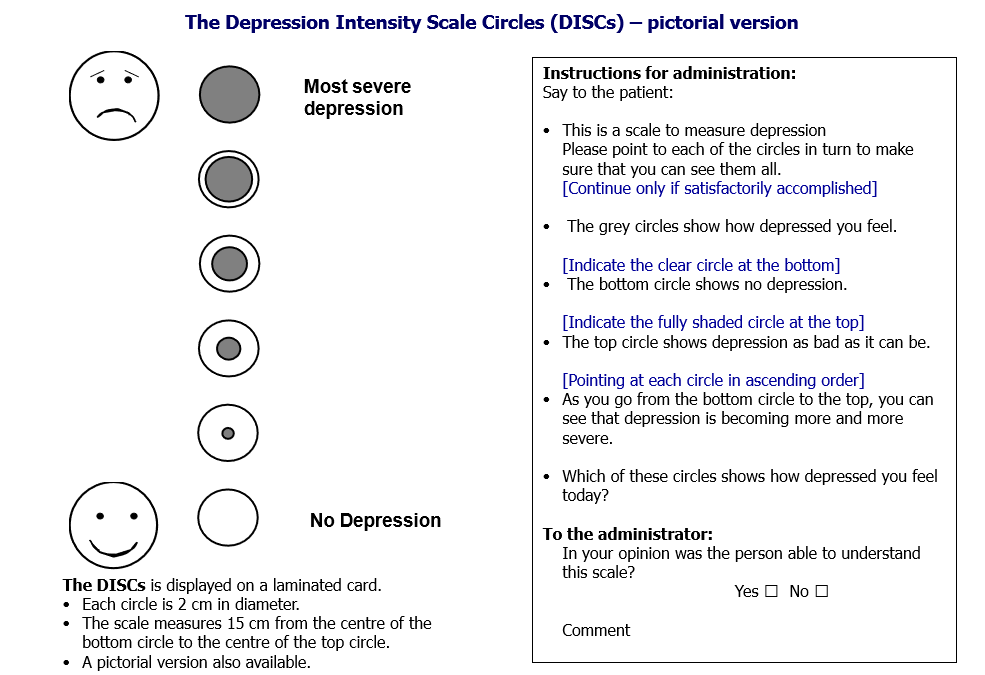
The Depression Intensity Scale Circles (DISCs): See below [1]
Communication
Being gentle and honest is key and there are many things to get over to those with stroke as well as those close to the patient
- It is normal to be tearful and anxious in the early days and weeks after a stroke
- It is normal to be frustrated and angry
- Most patients have coping skills that will help them
- We are here to help and support with words and helping to plan the future and also medications if needed
- Use a mood questionnaire to give quantitfiable numbers which can be repeated later
- If depressed ask about suicidal ideation gently
Emotionalism
Not uncommon after a stroke and can lead to laughing or crying for no apparant reason. The crying or laughing may be inexplicable and may not represent true feelings. However it tends to occur when there are situational emotional environmental triggers.
Mood Pathway
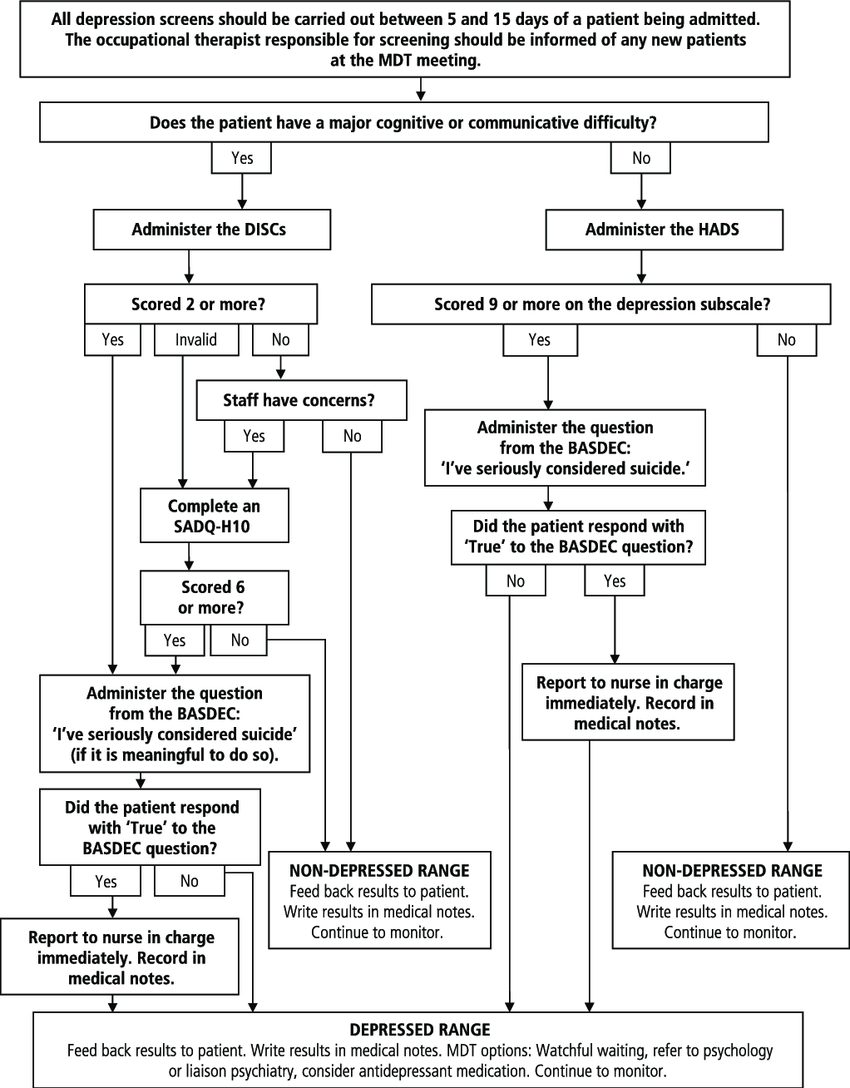
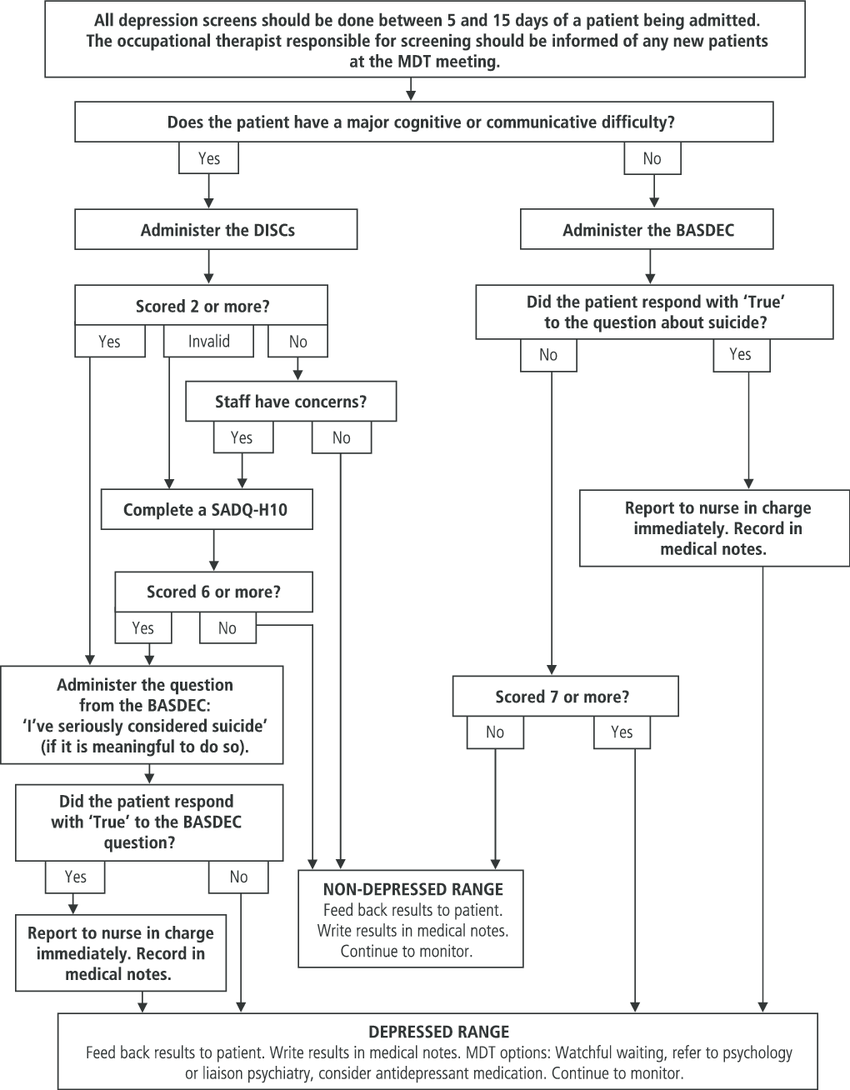
A pathways for screening for post-stroke depression [2] was developed. It was made clear that patients should be screened within 5-15 days of admission with an item to indicate suicidal ideas and to manage the likely outcomes would be: referral on, watchful waiting, medication.
Patients under 65
Patients over 65
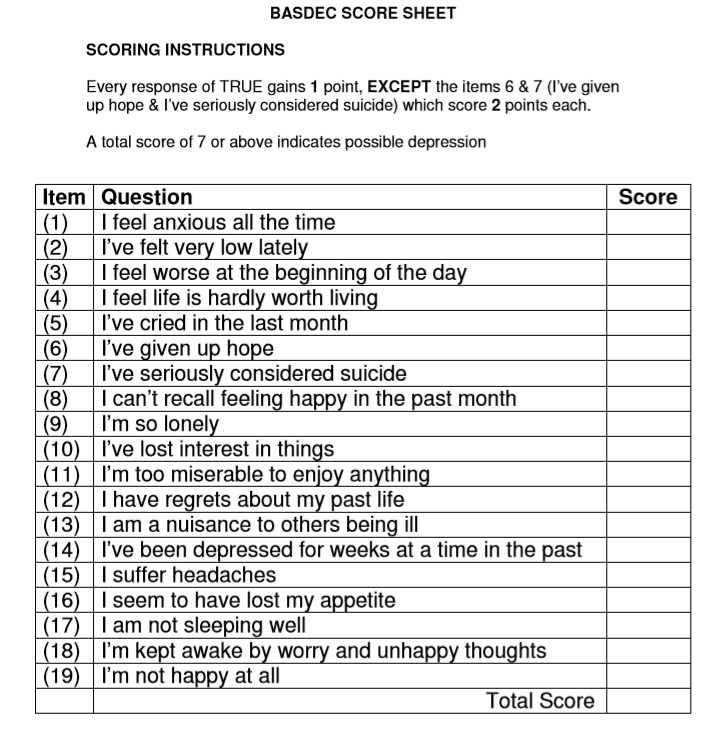
BASDEC
SADQH10
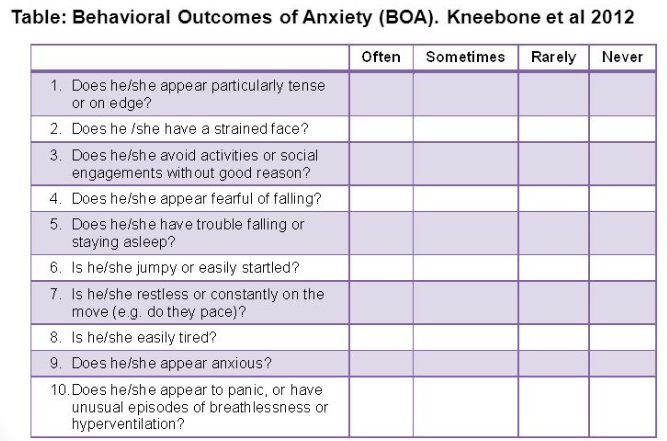
The Stroke Aphasic Depression Questionnaire (SADQ-10) can be used with people with communication difficulies and takes 10 minutes
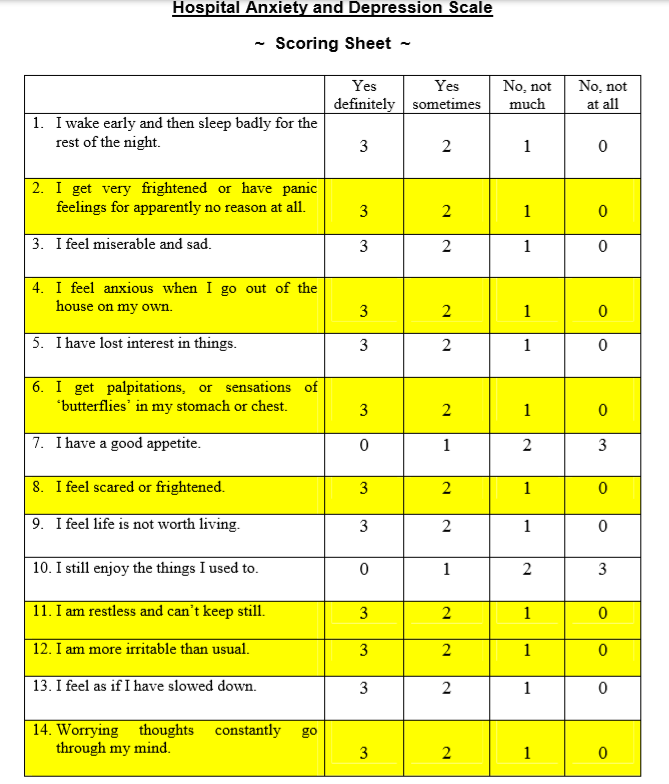
Hospital Anxiety and Depression Scale (HADS)
The Hospital Anxiety and Depression Scale (HADS) was devised 30 years ago by Zigmond and Snaith [1] to measure anxiety and depression in a general medical population of patients. The beauty of the HADS score is its simplicity, speed and ease of use. The questionnaire was historically freely available.
PHQ-9. (10 minutes).
Verbal people can be assessed with the PHQ-9. (10 minutes).
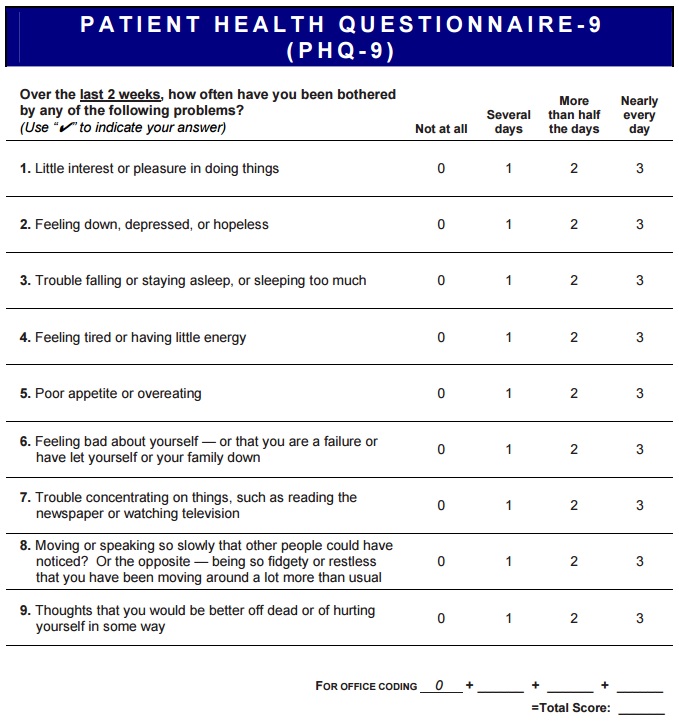
Depression Severity: 0-4 none, 5-9 mild, 10-14 moderate, 15-19 moderately severe, 20-27 severe.
Staff Training
To enable good mood screenign it is important to educate staff about depression; nature, signs, consequences and treatments. It is key to demonstrate the clinical value of screening in terms of helping patients and families. Inform more staff about guidelines. Train and empower more staff to screen. Develop screening resources (tests). Allow more staff time to screen. Support screening from the top. Make screening for depression a routine assessment. Monitor outcome and support staff to improve outcome further
Relationships after stroke
Relationships can change after stroke. Both the patient and the partner will come awaty from stroke with their own particular hopes and fears. Stroke changes many things. Self image is certainly soemthing that can be altered and many of us live in a false view of personal indestructibility and stroke shatters that and brings us to the truth that life can and is fragile but that it goes on. Stroke can have fundamental effects in terms of employment, financial income and worries. Thre may be children and not just a spouse who are affected.
Sex After stroke
This is a subject which many find difficult to discuss and avoid but we must consider it in those who want to have normal active sexual activity after stroke. Stroke affects all ages. For some patients it may not be relevant but the should at least be offered advice. Sex is often a source of anxiety in normal life, body image, desire, mood, self-esteem, fatigue, pain, spasticity, catheters and continence issues and libido are all complex topics. Some worry that sex may cause another stroke. This is rare indeed and the only association is with subarachnoid haemorrhage and aneurysm which if treated by coiling or clipping should make any risk very low indeed. It is otherwise very rare for sex to cause stroke. Regaining normal sexual relationships may take time and experimentation to get things right. Begin slowly and be realistic in terms of time and success so as not to cause disappointment. Initially the goals should be intimacy rather than orgasm. Finding a comfortable position. Often gravity neutral positions such as side by side is easiest with less fatigue. It can take time and patience to regain previous form or find a new sexual life that couples can explore and enjoy. Other issues may include impotence and low libido. Some drugs used can cause impotence. Viagra and other drugs may be used but are usually not prescribed for several months after stroke. Again, the general practitioner is useful and may be able to help.
Management
- Providing timely sympathetic and patient centred information on the current situation and the future providing hope and better days ahead where possible. Often needs multiple discussions. Keep them short. Make 1-2 points and then revisit at another day or time. Involve close family or those important to the patient. Have a coherent message. Involve speech therapy if dysphasic. Assess cognition an ensure messages take any cognitive issue sinto account. Mood screenign is a current part of SSNAP which can help to raise its profile and importance.
- Cognitive-behavioural treatments.
- Medications may help
References
- [1] Turner-Stokes L, Kalmus M, Hirani D, Clegg F. The Depression Intensity Scale Circles (DISCs): Initial evaluation of a simple assessment tool for depression in the context of brain injury . Journal of Neurology, Neurosurgery and Psychiatry 2005;76:1273-8.
- [2] Implementing a mood pathway Dr Ian Kneebone Consultant Clinical Psychologist & Visiting Reader
| Note: The plan is to keep the website free through donations and advertisers that do not present any conflicts of interest. I am keen to advertise courses and conferences. If you have found the site useful or have any constructive comments please write to me at drokane (at) gmail.com. I keep a list of patrons to whom I am indebted who have contributed. If you would like to advertise a course or conference then please contact me directly for costs and to discuss a sponsored link from this site. |