Learning objectives
|
Introduction
- A Dural AV Fistula is a shunt from a dural artery (meningeal or occipital) to a dural venous channel
- These are acquired deficits not congenital like AVMS and potential cause of ICH and SAH
- 10 % of all intracranial AVMS. Most common in females > males
Aetiology
- Causes include head injury, open surgery and Cerebral venous sinus thrombosis.
- These "fistulae" are extra axial direct connections between arterial flow and dural venous sinuses.
- The result is flow, shunting, pressure effects and venous congestion and haemorrhage.
- They lie within the dura mater most commonly with the transverse sinus
- Carotid-cavernous sinus shunts cause chemosis and scleral injection and an audible bruit.
- Lesions without cortical venous reflex almost never cause neurological deficits
Sites
- Cavernous sinus behind the eye: chemosis, reduced acuity, bruit, swelling of the eye.
- Transverse/sigmoid sinus behind ear: pulsating noise (tinnitus). Stroke like symptoms, seizure like activity, headaches.
- Vertebral artery
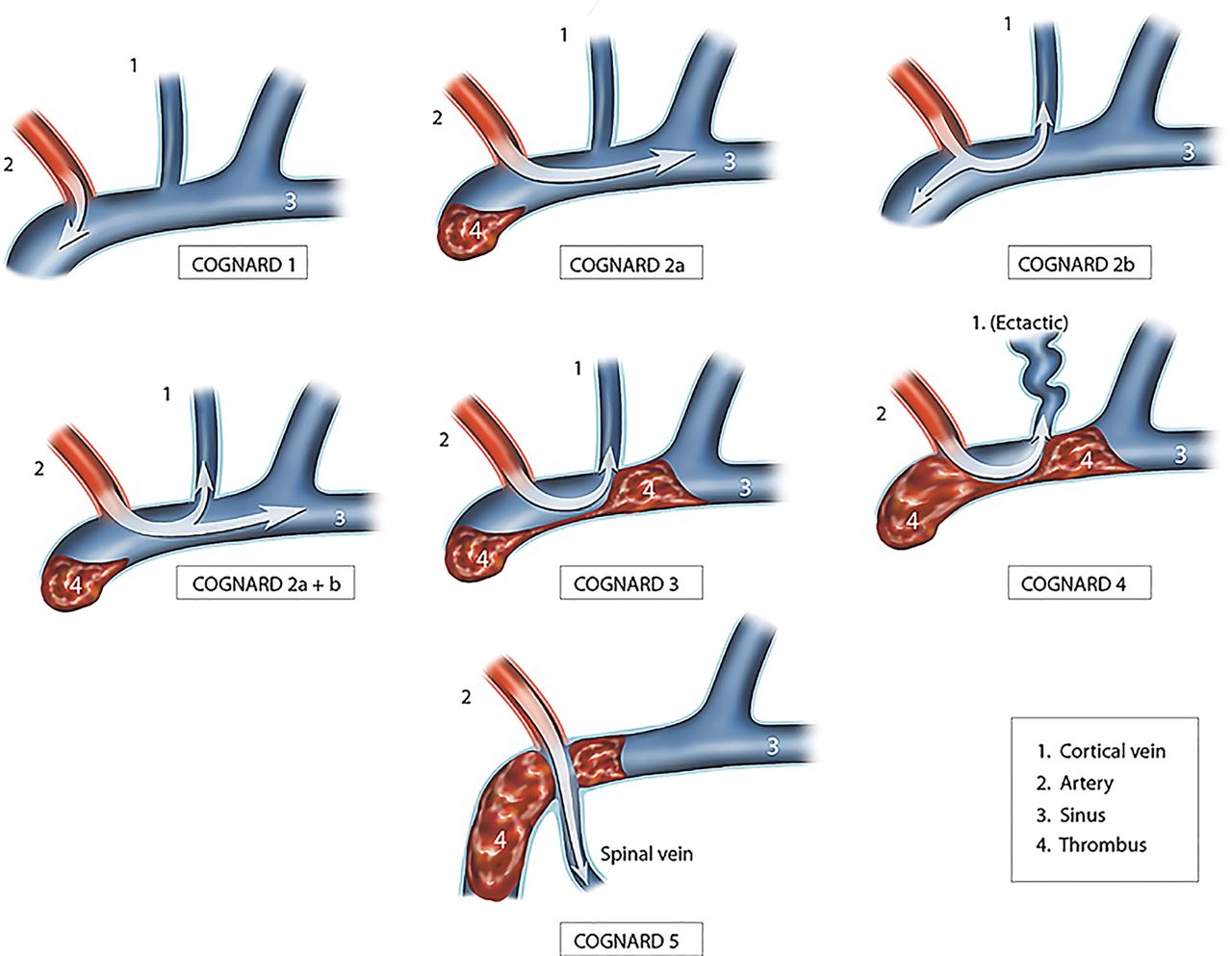
Classification
Clinical
- Possibly asymptomatic, Dural pain fibres can lead to headache.
- Seizures, bruits, headaches, stroke like episodes
- Signs of increased intracranial pressure and bleeding.
Investigations
- Diagnosis is by Angiography - CTA/MRA/DSA. There is usually localised venous congestion with dilated cortical veins and vasogenic oedema. Angiography demonstrated early venous filling with arterial supply from external carotid artery branches.
Management
- Annual bleed risk is difficult to determine but felt to be less than 5% per annum.
- Treatment options include conservative, endovascular embolisation using N-butyl-cyanoacryalate glue or other substance or surgery.
Last updated: 18/11/2018
| Note: The plan is to keep the website free through donations and advertisers that do not present any conflicts of interest. I am keen to advertise courses and conferences. If you have found the site useful or have any constructive comments please write to me at drokane (at) gmail.com. I keep a list of patrons to whom I am indebted who have contributed. If you would like to advertise a course or conference then please contact me directly for costs and to discuss a sponsored link from this site. |