Learning objectives
|
Introduction
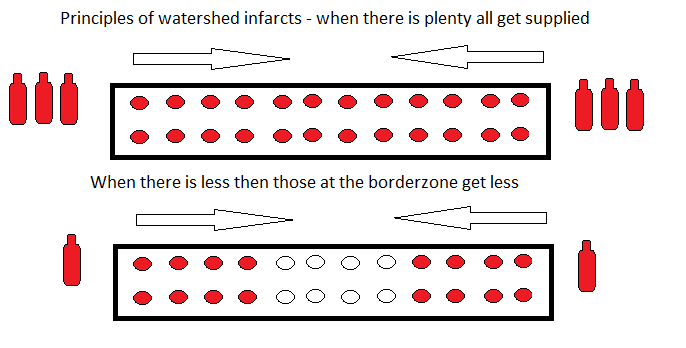
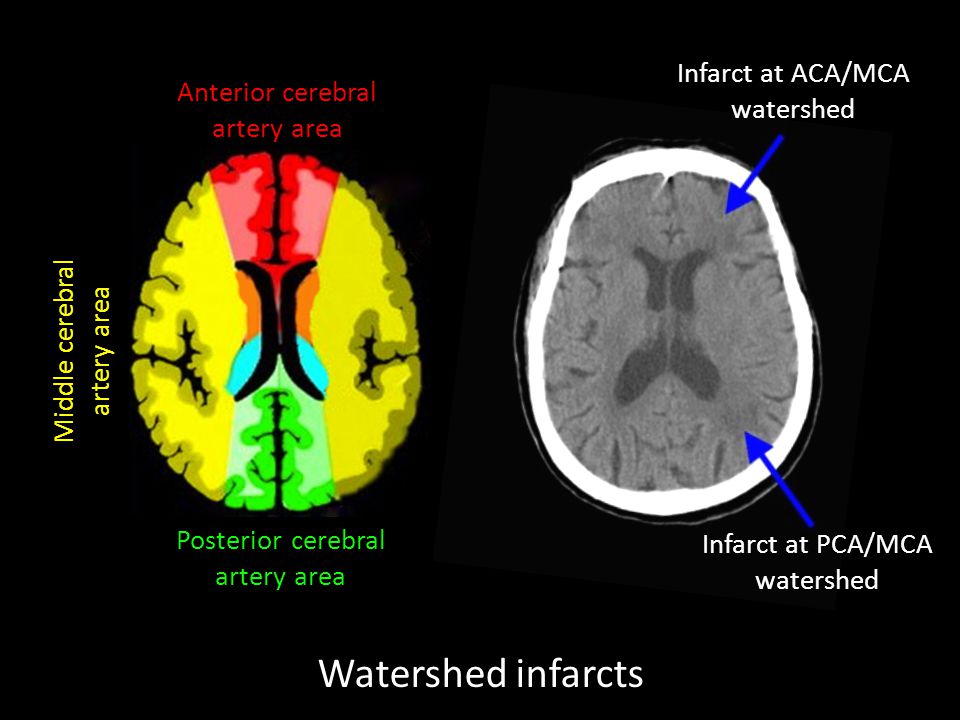
A watershed infarct is a stroke caused by a drop in circulating pressure and or volume that results in critical ischaemia or infarction between territories. Classically between MCA and ACA or MCA and PCA. The actual blood stream blockage/restriction site can be located far away from the infarct.
Aetiology
How to explain. If you and friends go out for dinner to a restaurant at a table for 20 people and the waiter places 3 bottles of wine at each end then as everyone pours a glass and passes it on everyone should get a drink. If however on another night you can only afford 1 bottle at each end of the table then those in the centre will find that the bottle is empty by the time it gets there. This is the watershed area and can in the brain be a line of infarction. It only happens when there is a generalised reduction in blood flow and the areas at the edges of any territory will get the least. One cause may be global drop in BP during sepsis or other causes of shock or during surgery or an occluded or critically stenotic ICA which supplies ACA and MCA and so this is where infarction is worst. The important issue is that the cause may be significantly proximal to the infarct such as a severely stenotic carotid or systemic hypotension.
Epidemiology
Border zone infarcts constitute approximately 10% of all cerebral infarcts
Images
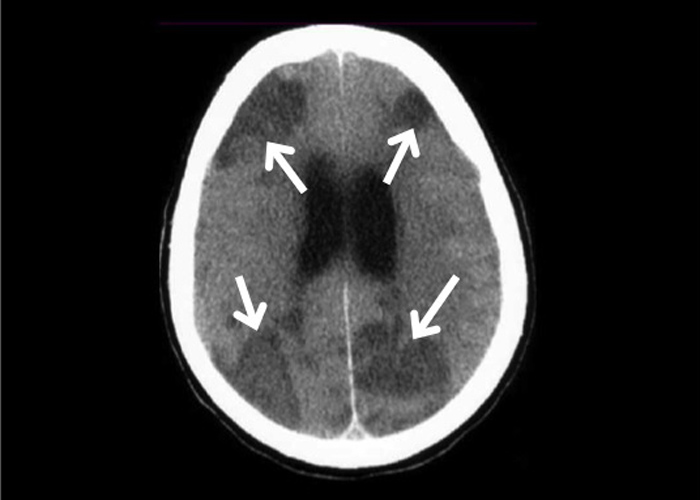
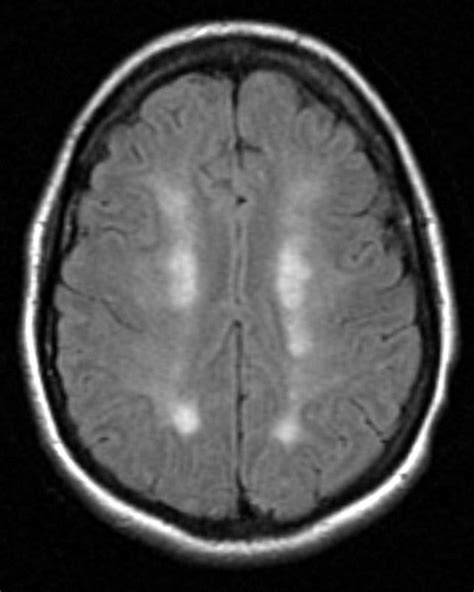
Classical rosary-like pattern in the centrum semiovale
Aetiology
- Arterial stenosis - may be multiple
- A Drop in systemic blood pressures
- A Drop in oxygen carriage - hypoxia, anaemia
- May be a role for microembolism
- Failure of cerebral autoregulation
- Increased demand
- Noncompetent circle of Willis.
- All or some of these
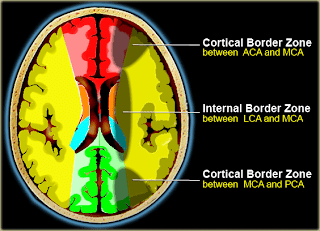
Classification
- External (cortical) regions
- Anterior - Middle cerebral artery : anterior external border zones and paramedian white matter
- Posterior - Middle cerebral artery : parieto-occipital areas
- Internal (subcortical) regions
- lenticulostriate–middle cerebral artery territories
- lenticulostriate–anterior cerebral artery territories
- Heubner–anterior cerebral artery territories
- anterior choroidal–middle cerebral artery territories
- anterior choroidal–posterior cerebral artery territories
| Misery perfusion represents a chronic failure of cerebral autoregulation associated with decreased cerebral perfusion pressures in the presence of extracranial and intracranial atheromatous disease. |
Locations
- Between ACA and MCA: in frontal cortex extending from anterior horn to the cortex
- Between MCA and PCA: in parieto-occipital region extending from posterior horn to the cortex
- Parallel parafalcine stripes in subcortical white matter at the vertex suggests profound hypoperfusion
Cerebellar Borderzone infarcts
- Border zone infarcts in the cerebellum are usually less than 2 cm in size
- Seen at the borders of the anterior inferior cerebellar artery, superior cerebellar artery, posterior inferior cerebellar artery, and their branches
Clinical
- May be episodic, fluctuating, or progressive weakness of the hand
- May be occasionally associated upper limb shaking
- Syncope, hypotension, and episodic fluctuating
- Progressive weakness of the hands are also supportive of this theory of hemodynamic failure
Investigations
- FBC, U&E, ABG if needed
- CT/MRI can define infarct and one may even see the classical rosary-like pattern in the centrum semiovale on MRI.
- Carotid duplex for ICA stenosis
- CTA for intracranial stenosis
- Exclude causes of hypotension e.g. MI ECG/Troponin, PE Dimer/CTPA
- Cerebral Perfusion scanning may be appropriate in some cases
Differential
- Embolic infarcts
- Localised intracranial stenosis
- Vasculitis
Management
- Identify cause if possible
- Caution with lowering BP
- Surgical referral for ICA stenosis
References
- The Pathophysiology of Watershed Infarction in Internal Carotid Artery Disease. Stroke. 2005;36:567–577
- Border Zone Infarcts: Pathophysiologic and Imaging Characteristics. Rajiv Mangla, MD • Balasubramanya Kolar, MD • Jeevak Almast, MD Sven E. Ekholm, MD, PhD RadioGraphics 2011; 31:1201–1214 • Published online 10.1148/rg.315105014 • Content Code
Last updated: 11/01/2019
| Note: The plan is to keep the website free through donations and advertisers that do not present any conflicts of interest. I am keen to advertise courses and conferences. If you have found the site useful or have any constructive comments please write to me at drokane (at) gmail.com. I keep a list of patrons to whom I am indebted who have contributed. If you would like to advertise a course or conference then please contact me directly for costs and to discuss a sponsored link from this site. |