|
Introduction
Thrombophilia is the 'love of thrombosis' and infers a clinical state in which there is a predisposition to thrombus formation almost always a venous thrombosis. Thrombophilia may be inherited or acquired. Acquired causes include illnesses such as SLE, Antiphospholipid syndrome and thrombocythaemia, polycythmaemia, macroglobulinaemia, nephrotic syndrome as well as malignancies and sickle cell disease. There really is a lack of good evidence to demonstrate a true association of ischaemic stroke and the inherited thrombophilias despite the common practice for these test to be requested in stroke work up in younger patients. This includes those with PFOs. The association between inherited thrombophilias and arterial stroke if there is one is weak and often affected by other prothrombotic risk factors. Ordering tests with little thought can lead to poor management and even inappropriate anticoagulant usage in these patients [Morris et al. 2010]. One in 7 patients with first-ever acute ischaemic stroke will test positive for one of the inherited thrombophilias, but the relation is likely to be coincidental rather than causal in almost all cases [Hankey GJ 2001]
Inherited thrombophilias are due to gene mutations affecting the procoagulants or anticoagulants which balance intrinsic haemostatic and fibrinolytic mechanisms. A genetic "loss of function" defect in an intrinsic anticoagulant or increased function in a procoagulant can upset the normal balance towards thrombosis. Procoagulant Clotting factors II,V, VIII and IX and XI. Anticoagulant factor antithrombin, Protein C, S and Z. Defect may lead to both venous or arterial thrombus formation [Green D 2003]. Gain of function mutations include the factor V Leiden (FVL) and the prothrombin gene 20210 A/G (PGM) mutations.
| Effect | Factors | Effect of loss of function |
|---|---|---|
| Procoagulants | Factor II, V, VIII, IX, XI | Propensity to Bleeding |
| Anticoagulants | Antithrombin, Protein C, S, Z | Propensity to Thrombosis |
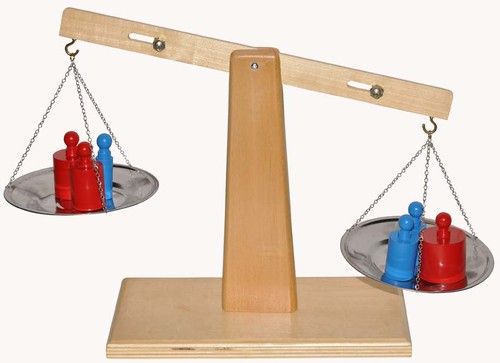
Thrombosis and Thrombolysis is a balance
If one were to try and evaluate prothrombotic risk estimation then it would be have to be balanced as below. It is important to note that a genetic predisposition may be additive to other temporary or permanant risks. A clinical picture needs to assess all the risks together. It may be that once a transient risk falls e.g. such as at the end of the post partum period that thrombotic risk returns to a low risk and lifelong anticoagulation may then not be needed and may indeed be more dangerous than the thrombophilia itself. Risks need to be reviewed when situations change.
Risk of Thrombosis = Procoagulants/Anticoagulants factors + Other Factors e.g. Immobility, Smoking, Pregnancy, Post op, OCP etc.
Inherited/Congenital Defects
Heritable thrombophilias increase the risk of venous (but not arterial) thrombosis. They are present in about 5% of the population, but most carriers never experience a deep vein thrombosis or pulmonary embolism. The antiphospholipid syndrome is also not included, because it is an acquired rather than a heritable thrombophilic disorder.
Incidence
| Name | Frequency |
|---|---|
| Factor V Leiden mutation | 3-7% |
| Prothrombin gene mutation | 1-2% |
| Antithrombin deficiency | 3 |
| Protein C deficiency | 0.3% |
| Protein S deficiency | 0.1% |
Factor V Leiden (FVL) mutation
Found in 5% of Caucasians. The mutation in the Factor V gene means Factor V Leiden as it is called is now more difficult to break down. There is increased thrombin generation and prothrombosis. The absolute risk, however, is low, with only 5% of such people developing an episode of VTE by age 65 years. No real association demonstrated with arterial disease but 3-5 fold increase in VTE for heterozygoes but 10 fold for homozygotes but these are rare. There may be a multiplicative effect with other risks such as use of the OCP but the absolute risk is still low. It is a weak risk factor for stroke. Stronger association in children with ischaemic stroke. Testing for FVL should be only in those under 40 as it becomes less relevant with age
Prothrombin 20210 Gene Mutation
Seen in 1-3% of Europeans. A mutation in promotor of prothrombin gene at position 20210 increases prothrombin synthesis which parallels risk of venous thrombosis. There is a 2-4 fold increased risk of VTE. Prothrombin levels are increased by about 30% in heterozygotes and 70% in homozygotes. There is increased risk of Cerebral venous thrombosis especially when combined with OCP and smokers. Test in those under 45
Antithrombin deficiency
Antithrombin was previously called Antithrombin III. The heterozygote state leads to increased thrombin. The two main deficiency types result in either a Tpe 1 quantitative defect or Type II defect. Type 1 is rare (0.02%). Heterozygote AT deficiency risk are unclear. Some estimate VTE risk as 5 fold.
Protein C, S and Z deficiency
These factors are anti-thrombotic and are Vitamin K dependent glycoproteins synthesised in the liver. They inhibit thrombosis and so any deficiency becomes theoretically prothrombotic.
- Activated protein C inactivates clotting factors Va and VIIIa as described previously. If there is heterozygous (partial with levels 20-30% normal) Protein C deficiency then there is increased DVT but CVT is rare even in the young.
- Protein S is a cofactor for Protein C. Protein S deficiencies may be acquired and seen with sepsis or aAPL syndrome or pregnancy. There is an association with protein S deficiency and CVT and arterial thrombosis.
- Protein Z has similar anticoagulant properties and is Vitamin K dependent. Mixed literature but likely not a risk factor for ischaemic stroke in young adults.
Acquired Defects
Heparin induced thrombocytopenia with thrombosis(HITT)
This is a prothrombotic disorder associated with heparin exposure that can lead to venous or arterial thrombosis. The blood tests show a falling platelet count and management is to immediately stop all heparin and switch to alternatives
Antiphospholipid syndrome
References
- Diagnosis and management of heritable thrombophilias BMJ 2014; 349 doi: https://doi.org/10.1136/bmj.g4387 (Published 17 July 2014)
- Guidance for the evaluation and treatment of hereditary and acquired thrombophilia
| Note: The plan is to keep the website free through donations and advertisers that do not present any conflicts of interest. I am keen to advertise courses and conferences. If you have found the site useful or have any constructive comments please write to me at drokane (at) gmail.com. I keep a list of patrons to whom I am indebted who have contributed. If you would like to advertise a course or conference then please contact me directly for costs and to discuss a sponsored link from this site. |