Learning objectives
|
About
The artery of Percheron was first described in 1973 by French Neurologist Gerard Percheron. It is interesting as it is an artery that provides vascular to two paramedian structures as most brain end arteries respect the midline and do not supply bilateral structures. It can produce a classical clinical presentation as seen below.
Pathophysiology
- This is a single vessel that supplies bilateral structures.
- Usually there are bilateral medial thalamic infarcts and perhaps involvement of midbrain
- May have altered mental status, vertical gaze palsy, and memory impairment
- Reduced awareness and coma likely as thalamus is the top of the reticular activating system
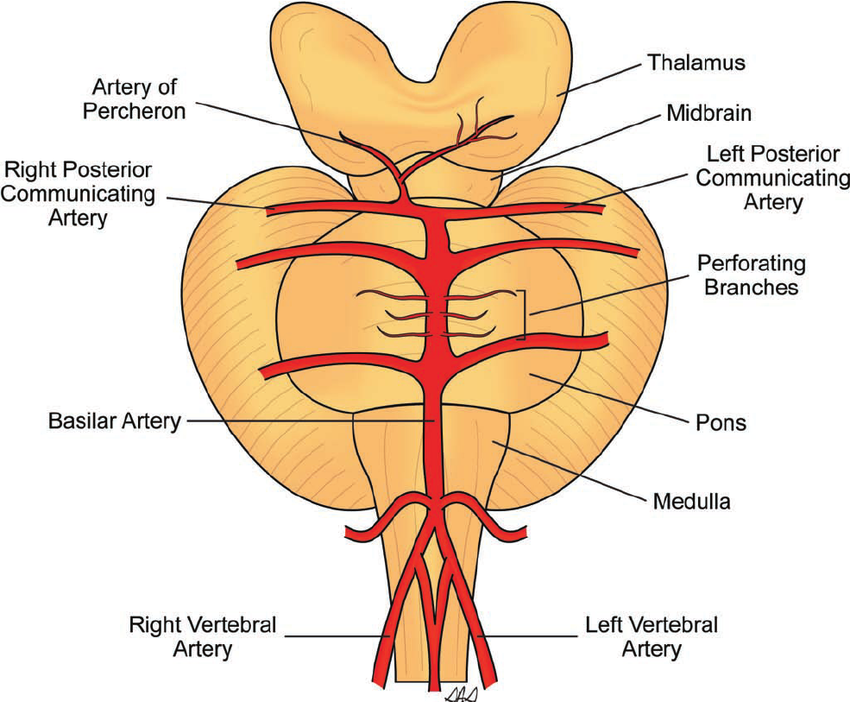
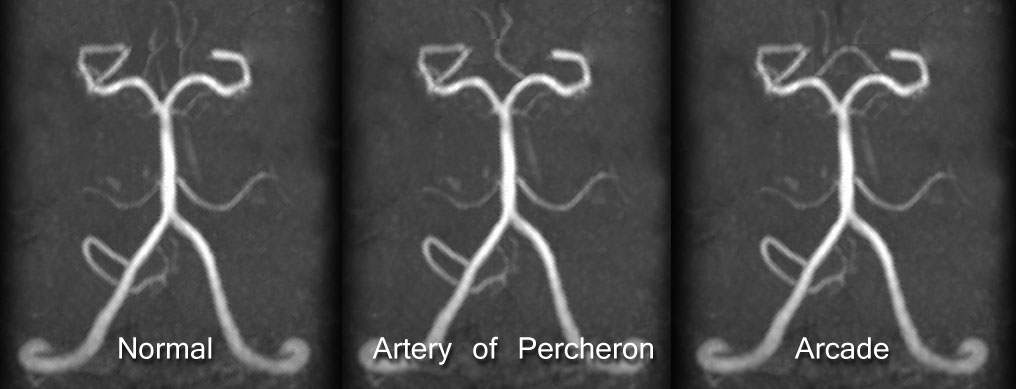
Anatomy of AOP
Usually there is an artery on either side supplying the right and left medial thalamus. Note there is an error in the graphic so read Posterior cerebral artery and not posterior communicating artery.
Epidemiology
- Acute Artery of Percheron infarcts represent 0.1 to 2% of total ischaemic stroke
- A typical stroke centre with 1000 strokes per annum may see 1-2 cases per annum
Aetiology
The arterial supply of thalamus and midbrain is complex and is provided by perforating branches from the posterior cerebral artery and the posterior communicating artery. Many numbers of significant variations in vascular supply of thalami and mesencephalon are seen. The Artery of Percheron is a vascular variant in which a single dominant thalamo-perforating artery arises from one P1/2 segment of PCA and bifurcates to supply both paramedian thalami. Occlusion of this vessel results in a characteristic pattern of bilateral paramedian thalamic infarcts with or without mesencephalic infarctions. Aetiology is likely cardioembolic or artery to artery from aorta or vertebral
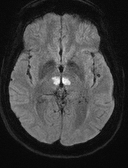
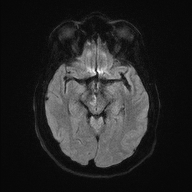
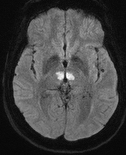
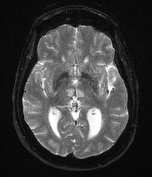
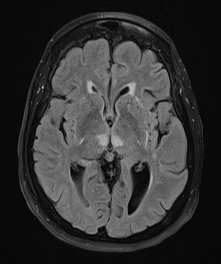
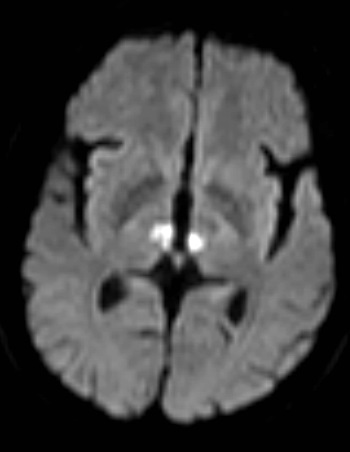
MRI appearance
 |
 |
 |
 |
 |
 |
Clinical
- Result of bilateral damage patient is unresponsiveness and acute coma.
- Somnolescence - patient is unresponsive but may roll over and pull up bed clothes as if sleeping.
- Coma in others even needing intubation.
- Pinpoint pupils may be seen unless IIIrd nerve involved
- Long term when awakens memory and cognition often affected
- Midbrain involvement - may have hemiplegia, IIIrd nerve deficits
Differentials in Comatose patient with normal initial CT
|
Investigations
- FBC, U&E, LFTs. CRP. ESR. Cholesterol
- ECG/24 hr tape for AF / PAF
- Echo for cardioembolic causes
- CT: usually normal but may show bilateral thalamic hypodensity with time
- MRI: classical bilateral "butterfly" medial thalamic infarcts and may show some midbrain involvement. There may be the V sign of a hyperintense signal intensity on axial FLAIR and DWI images along the pial surface of the midbrain in the interpeduncular fossa in 67% in cases of AOP infarction with midbrain involvement.
- CTA/MRA to look for vertebral dissection can be useful as a cause
- LP may be normal mildly elevated protein but may help exclude infective process if suspected
Management
- ABC, support acutely. Often delayed diagnosis as stroke as other non stroke diagnoses need exclusion
- Consider thrombolysis and /or thrombectomy if appropriate. However often the presentation is difficult and diagnosis delayed and beyond window for thrombolysis.
- Uncertainty means that one may give antibiotics, antivirals initially as ?? Meningitis/Encephalitis. LP may be normal or mildly elevated protein.
- Can make good recovery. But there may remain memory and cognitive issues.
- Manage as other ischaemic strokes. Look for embolic sources.
- Standard Care: Antiplatelets, BP medications, Statin
- Neurorehabilitation: cognitive issues may predominate so involve Neuropsychology
References
- Jeremy D. Schmahmann. Vascular Syndromes of the Thalamus
- Artery of Percheron Infarction: Imaging Patterns and Clinical Spectrum
Last updated: 18/11/2018
| Note: The plan is to keep the website free through donations and advertisers that do not present any conflicts of interest. I am keen to advertise courses and conferences. If you have found the site useful or have any constructive comments please write to me at drokane (at) gmail.com. I keep a list of patrons to whom I am indebted who have contributed. If you would like to advertise a course or conference then please contact me directly for costs and to discuss a sponsored link from this site. |