Learning objectives
|
Introduction
- Cerebral cavernous malformations are the most common vascular malformations
- They are formed as a collection of abnormal blood vessels which can bleed, and this may extend beyond its fragile walls.
- Cavernomas may be seen in 0.1-0.5% of the population and some have a genetic basis.
- They are commoner in Hispanic communities (especially Mexican-American).
Pathophysiology
- There is no large feeding artery or large draining vein.
- They can be found anywhere in the cerebrum, brainstem or cord
- The deep situated lesions tend to bleed more than superficial.
- Genetic variants CCM1, CCM2, and CCM3, found on the 7q, 7p, and 3p chromosomes, respectively
Clinical
- Clinical presentation includes silence or presentation with intracerebral haemorrhage
- Focal Seizures, focal neurology or raised ICP, Headaches or Hydrocephalus.
Cavernomas in the midbrain
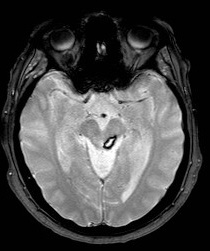 |
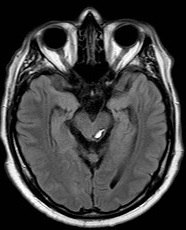 |
Investigations
- CT or MRI may show a "raspberry or popcorn like" Cavernoma +/- associated haemorrhage.
- MRI SWI or GRE is the modality of choice and will show blood products well.
- It is not well seen on a cerebral angiogram called "angiographically occult"
| Type | Radiological findings |
|---|---|
| Type 1 | hyperintense on T1- and T2-weighted imaging due to a hemosiderin core from subacute haemorrhage. |
| Type 2 | loculated haemorrhages enveloped by gliotic tissue, presenting as a mixed signal on both T1 and T2 sequences. On T2 imaging, type II lesions also have a hypointense rim, resulting in the “popcorn” appearance |
| Type 3 | presence of an isointense core, indicating chronic resolved haemorrhage, typically seen in familial CM |
| Type 4 | small malformations that can only be seen in gradient recalled echo (GRE) MRI as hypointense foci and are thought to be capillary telangiectasias |
Management
- Microsurgical resection, stereotactic radiosurgery, and conservative management
- Indication include after a bleed, intractable seizures or neurological dysfunction, Depends on location e.g. great care in highly eloquent areas such as brainstem where a conservative approach is taken. Surgical management of particular brainstem cavernomas is controversial.
- There is some evidence that resection of brainstem cavernomas is the treatment of choice in the majority of these cases because of the high incidence of morbidity related to one or often several brainstem haemorrhages. [Madjid S et al 2001]
- May be managed conservatively and followed by yearly MRI scans
References
| Note: The plan is to keep the website free through donations and advertisers that do not present any conflicts of interest. I am keen to advertise courses and conferences. If you have found the site useful or have any constructive comments please write to me at drokane (at) gmail.com. I keep a list of patrons to whom I am indebted who have contributed. If you would like to advertise a course or conference then please contact me directly for costs and to discuss a sponsored link from this site. |