Themes: Hyperacute Care, SAH, Complications.
| Mary is a 56 year old lady who presents with the sudden onset of a severe headache whilst taking the clothes off the washing line. She describes it as the "worst headache that she ever experienced". Like being hit with a cricket bat. She thinks she passed out for a short period of time as she woke up on the floor with bruises. She was found on the floor by her daughter who heard a bang as she fell. When you see her she is lying on a trolley in the ED. She feels terrible and is holding her head and lying on her side. You organise an urgent CT head. |  |
|---|
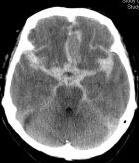
Brain Imaging: Non contrast CT head (axial)
1. What is the diagnosis
This is a subarachnoid haemorrhage which is a form of haemorrhagic stroke. You can the CT scan with blood seen throughout the subarachnoid space. It typically presents with a severe headache often called a "thunderclap" headache which becomes maximal very quickly and is often described as their worst headache ever. In over 99% of cases the CT scan will show blood in the subarachnoid space if done within 6 hours. These patients don't usually come to the stroke unit as they go under the care of neurosurgery to exclude an aneurysm that needs treatment. The stroke team however may be the first to see them and so need to both recognise the diagnosis and contact the neurosurgeons.
2. What are the commonest causes of this type of stroke.
Commonest cause of SAH is the rupture of a berry or saccular aneurysm. Blood leaks at arterial pressures. This causes an instant and terrible headache. Some patients may pass out initially. A saccular aneurysm is a weakness in the blood vessels and can leak during exertion - running, coitus, lifting weights or hanging out the washing or some drugs that suddenly raise BP such as cocaine.
- Berry/Saccular aneurysm
- Arteriovenous malformation
- Unknown causes in some
3. What are the next steps ?
- As ever ABC is important and some patients may drop GCS and need intubated and ventilated.
- Neurosurgical referral is needed as the main risk is rebleeding from an aneurysm
- Patients go to ITU under neurosurgery and not the HASU
- Neurosurgeons or Interventional neuroradiologsist can treat any aneurysm
- This reduces the risks of rebleeding
- Patients often go to Neuro ITU first for invasive monitoring and control of BP
4. She is given Nimodipine. What does Nimodipine do ?
Nimodipine is a calcium channel blocker that reduces the risk of vasospasm which is often seen in the days after an aneurysmal SAH and can result in an ischaemic stroke. For patients presenting with aneurysmal subarachnoid hemorrhage (aSAH), nimodipine 60 mg given by mouth every 4 hours should be started within 96 hrs of the presumed onset of the aSAH and continued for 21 days
5. What will the neurosurgeons do ?
- Angiography (DSA) to detect the source of the bleeding usually a berry aneurysm
- Treat the aneurysm either with clipping or coiling it
- Coiling is done by neurosurgeons or interventional neuroradiologists
- Clipping is done by neurosurgeons
- Treat any associated complications e.g. hydrocephalus
6. What are the most worrying complications ?
- Rebleeding causing further disability and even death
- Vasospasm causing an ischaemic stroke
- Seizures needing anticonvulsants
- Hyponatraemia
7. What is the cause of Hyponatraemia
In most cases it is renal Na loss (Naturiesis) and not SIADH but check for both using urine and serum osmolality and measuring urinary Na. For those with renal Na loss then replacement is needed. If SIADH is the cause then fluid restriction is required.
There is more information at SAH article.
Next: >> Clinical Scenario 7: next
| Note: The plan is to keep the website free through donations and advertisers that do not present any conflicts of interest. I am keen to advertise courses and conferences. If you have found the site useful or have any constructive comments please write to me at drokane (at) gmail.com. I keep a list of patrons to whom I am indebted who have contributed. If you would like to advertise a course or conference then please contact me directly for costs and to discuss a sponsored link from this site. |